
2025 Wrap-Up: Growth, Progress, and Challenges
Published to the Blog
January 30, 2026
Summary
In 2025, we achieved remarkable growth through international expansion, dramatic improvements in cost-effectiveness, and major platform enhancements, while also deepening our understanding of the challenges in measuring our impact.
Expansion to a new country: We launched Newborn Care Foundations in Zambia in October, reaching over 30,000 completions by year-end (more than 65% of all nurses and midwives in the country), bringing total 2025 completions to 54,705 across Nigeria and Zambia.
Declining unit costs increased our cost-effectiveness: Our philanthropic cost per course completion dropped from $14 in 2024 to close to $2 in 2025, and updated modeling suggests the program may be well above GiveWell’s bar for highly cost-effective programs.
Platform improvements enabled growth: Key platform achievements included improvements to performance and user experience, over 99.9% uptime, new sharing features, partner dashboards for real-time data, and successful advertising campaigns costing under $1 per trainee.
Ongoing impact uncertainties: While we're increasingly confident in the cost-effectiveness of the program, key uncertainties remain around the course's effect on practice change, duration of that change, and effect of practice change on health outcomes.
Targeting further growth in 2026: Our plans include expanding the newborn care course to more countries, achieving 50,000 additional course completions, upgrading our impact evaluation methods, and launching at least one new course.
Growth and Expansion of Newborn Care Foundations
One of our key achievements in 2025 was the launch of Newborn Care Foundations in a second country. We worked closely with the Nursing and Midwifery Council of Zambia (NMCZ) and a Zambian pediatrician to create a locally adapted, government-approved version of the Newborn Care Foundations course. The course matches Zambia’s guidelines and cultural context, and is approved for 20 continuing professional development (CPD) points by nurses and midwives in Zambia. From launch day – October 8, 2025 – to the end of the year, more than 30,000 people in Zambia completed the course.
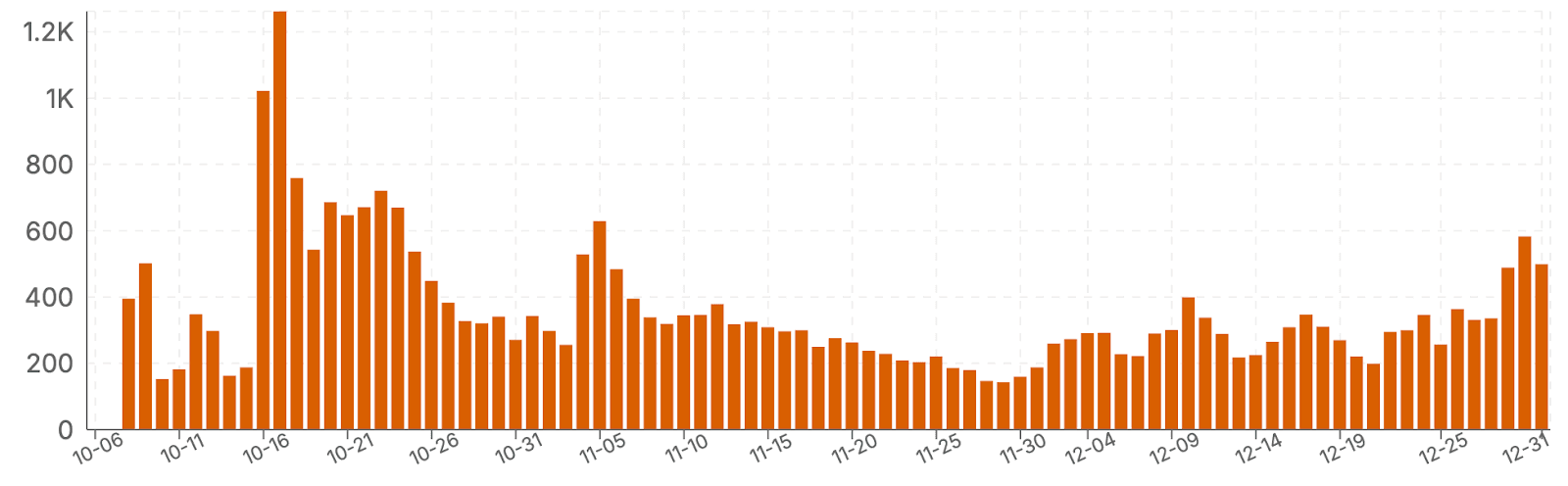
Daily completions of Newborn Care Foundations in Zambia from October 8, 2025 to December 31, 2025.
Over 85% of course completers reported being nurses or midwives, so we estimate that we reached more than 65% of the total population of nurses and midwives in Zambia in less than three months [1]. We believe key factors in the successful rollout of this course included:
A high degree of buy-in from local stakeholders, particularly NMCZ, leading to dissemination of the course through official channels,
Allocation of CPD, which motivates nurses and midwives to take the course (CPD is required for license renewal), and
Successful direct-to-health-worker advertising of the course through social media by the HealthLearn team.
In addition, across all of 2025, over 24,000 people in Nigeria completed the course, bringing total completions of Newborn Care Foundations in 2025 to 54,705. This is almost a 9-fold increase in course completions relative to 2024. Learning gains, measured with a matched pre- / post-course test, were comparable in Zambia (22 percentage point increase) to those in Nigeria (19 percentage point increase), suggesting quality has not deteriorated in spite of substantial program scaling.
Improvements to our Platform and Scalability
Key upgrades to our learning platform and our outreach to learners also enabled this massive growth. We updated the platform to improve performance and the user interface, and we maintained over 99.9% uptime throughout 2025, ensuring a consistent and high quality user experience. We also built new features that allow learners to voluntarily and securely share their course completion achievements with others and encourage them to take the course. By the end of 2025, sharing drove well over 10% of total course completions. Sharing has the added benefit of tapping into social enablers of long-term behavior change, so we’re excited about more growth in this area in the future.
We built new features that allow our NGO and government partners to access dashboards that display aggregated data on learner progress and learning within courses. This promotes transparency and real-time data insights while maintaining security and user data privacy.
Finally, we built our capacity to directly inform health workers about the free Newborn Care Foundations course. We tested several different marketing campaigns and channels throughout 2025, and we found that Facebook advertising was a particularly productive channel. These campaigns contributed to many thousands of course completions, with an average advertising cost well under $1 per course completer. The campaigns had the added benefit of bringing many learners to the platform who went on to take courses offered by our nonprofit partner, Resolve to Save Lives, pointing to the advantages of bundling multiple impactful and audience-aligned courses together on the same learning platform.
Assessing Program Impact
Building on the small-scale clinical evaluation and updated impact modeling that we completed at the end of 2024, we put substantial effort in 2025 towards improving our understanding of the impact of the Newborn Care Foundations course on health worker clinical practices and mortality outcomes.
Desk Research Supports Prior Impact Estimates
Our end-2024 impact model estimated the benefits that accrue from improving just one newborn care outcome: early initiation of breastfeeding. To follow up on that work, we published two white papers (summaries here and here) that delve into research on the causal relationships between early initiation of breastfeeding and newborn health outcomes. Together, these reports support our prior understanding that early initiation of breastfeeding directly promotes newborn survival, but this work did not substantially change our estimates of the effect size of this relationship. We still feel that the effect could be larger or smaller than the point estimates used in our end-2024 impact model. This research also increased our understanding of the complexities (discussed in more detail below) inherent to future evaluations of the Newborn Care Foundations course.
Higher Impact and Lower Uncertainty Through Scaling
The cost per completion of Newborn Care Foundations course dropped precipitously in 2025. Philanthropic cost per course completion, averaged over the year, was just over $2, compared with $14 in 2024. This number is calculated by subtracting earned (non-philanthropic) revenue from our total costs for the year, then dividing this by the total number of course completions [2]. Costs increased as our team grew in 2025, but this was outpaced by rapid growth in the number of health workers taking the Newborn Care Foundations course.
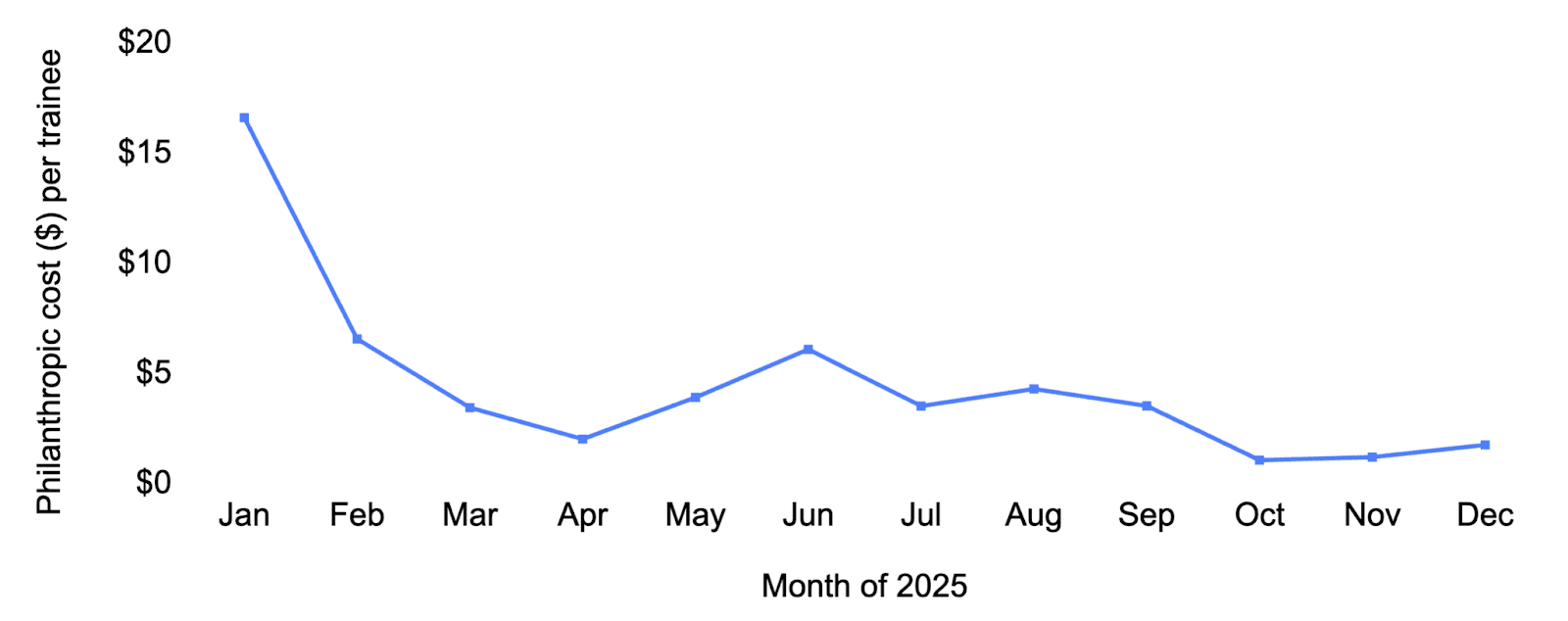
Philanthropic cost per Newborn Care Foundations trainee (course completer) on a monthly basis throughout 2025. Philanthropic cost per trainee was $2.26 averaged over the year.
The primary drivers of HealthLearn’s cost-effectiveness are impact per trainee and cost per trainee. While impact per trainee is challenging to quantify precisely, cost per trainee can be calculated directly from our platform analytics and financials. We can use this relationship to derive an updated back-of-the envelope estimate of program cost-effectiveness and impact. At the end of 2024, we estimated the program was 24 times more cost-effective than GiveWell’s benchmark [3]. Since cost per course completer was ~6.4-fold lower in 2025, this suggests the program is ~151 times more cost-effective than the GiveWell benchmark. We do not have new evidence that would support major revisions to our end-2024 estimate of impact per trainee, so we haven’t updated that aspect of the model. We therefore consider this new figure (151x) to be an approximate order of magnitude assessment rather than a literal point estimate of HealthLearn's cost-effectiveness in 2025 [4].
While the updated cost-effectiveness is an impressive number, we do have reasons to interpret it cautiously. Notably, rates of adherence to some of the key newborn care practices targeted in the Newborn Care Foundations course are higher in Zambia than in Nigeria, and newborn mortality is also a less common outcome in that country. It seems possible that the impact per trainee is substantially lower in Zambia, but even if we exclude all course completions in Zambia from our impact calculations, we still estimate the program is ~68 times more cost-effective than the GiveWell benchmark. If we focus only on completions in Nigeria and remove earned revenue from these calculations (e.g. we divide total costs for the year by total completions in Nigeria), the multiplier drops further to ~28x. We think this spread (28-151 times the GiveWell benchmark) represents a plausible cost-effectiveness range for the program.
Remaining Uncertainties; Reasons for Skepticism and Optimism
Improved unit costs make our team increasingly confident that HealthLearn is cost-effective, even in the face of uncertainty. It’s worth considering the most likely reasons the program might eventually prove to not be cost-effective, most of which would require no or vanishingly small benefit (impact) per trainee. In our view, the key uncertainties that remain are:
Effect size of the course on practice change: how much the course improves clinical practice [5].
Duration of practice change: how quickly any improvements in practice decay or revert back to the pre-course level.
Effect size of practice change on health outcomes: how much any given improved clinical practice reduces mortality.
Other factors that could reduce cost-effectiveness, but seem unlikely to negate benefits entirely, include costs that aren’t accounted for in our model, such as the cost of health worker time that goes towards taking our courses.
In our end-2024 evaluation, we applied large discounts to adjust for these uncertainties. While we still feel such discounts are justified, it is also possible that we discounted too heavily and the program is more impactful than our point estimates would suggest. There are some compelling reasons for optimism. In particular, the model doesn’t account for:
the effect of improving clinical practices or intrapartum outcomes other than early initiation of breastfeeding,
reductions in morbidity,
any secondary outcomes or knock-on benefits, or
the benefits of the other courses we host on the HealthLearn platform.
Evaluation Challenges
Our work on evaluation in 2025 made us more aware of the major challenges we face in arriving at more precise and accurate impact estimates. Notably, the minimum effect size required for the program to be cost-effective is so small that truly massive sample sizes (in the millions [6]) would be needed for a cluster randomized controlled trial that is powered to detect decision-relevant reductions in mortality. Moving forward, we aim to conduct further evaluations (and, as appropriate, desk research) to assess each of the key uncertainties identified above, with the mid-term goal of running a more rigorous experimental evaluation of the effect of the program on clinical practice. We’ve already piloted a new mother survey that we will now use to measure changes in early initiation of breastfeeding after the course is rolled out. We are also aiming to develop in-app or post-course assessments that can be delivered at scale and serve as valid proxies for clinical practice change.
Plans for 2026
Given the enormous growth we experienced in 2025, we believe 2026 is a particularly pivotal year. Our efforts this year are oriented towards sustaining program growth, preparing for further scaling, improving our impact estimates, and expanding impact by offering new courses.
Our 2026 goals are to:
offer the Newborn Care Foundations course in at least three countries,
have 50,000 additional people complete the Newborn Care Foundations course,
upgrade our evaluation to increase our confidence in the impact of the program, and
launch a new HealthLearn course in at least one country.
Please follow these links if you’re interested in working with us or supporting us.
Note: We updated this post between February 3-7, 2026 to reflect a range of possible cost-effectiveness multipliers for the program and to provide qualitative context for these multipliers.
[1] This is based on World Bank data indicating 2.1 nurses/midwives per 1,000 in population, and an estimated population of Zambia of 19.6 million, yielding an estimated >41,000 nurses / midwives in Zambia. Calculations can be found here.
[2] In addition to philanthropic revenue from grants and donations, HealthLearn earns revenue from hosting courses for another NGO. This calculation is done on a cash basis, so it does not incorporate certain accrual accounting considerations.
[3] At the time, this was expressed as multiples of the cash transfer benchmark. GiveWell has since updated its methodology, but the new benchmark is similar. We still use a pre-2024 baseline for these calculations to match the methodology of our previous BOTEC.
[4] The calculation supporting these estimates can be found here.
[5] Available evidence, including small-scale direct observation, supports improved clinical practice after taking the course. In 2025, we conducted a post-course survey in which a large majority of respondents reported seeing increased adherence to a key practice (early initiation of breastfeeding) in the facilities where they work. While this is consistent with practice change, we do not place great weight on those findings, given obvious concerns about desirability bias and related concerns with surveys.
[6] The program would be cost-effective if it reduced neonatal mortality by less than 1%. Detecting such a small reduction in a relatively rare event in a randomized controlled trial requires impractically large sample sizes. Back of the envelope calculations can be found here. It may be more feasible to measure clinical practice change in a randomized setting, and we are looking into that.
Join our email list to get occasional updates from us.