
What Complex Interventions Tell Us About Early Breastfeeding and Mortality
Published to the Blog
December 1, 2025
In earlier work, we concluded that early initiation of breastfeeding (EIBF) and immediate skin-to-skin contact (SSC) reduce neonatal mortality and can be improved with targeted interventions. We’ve now followed up with a review of “package” neonatal health interventions [1] in which EIBF rates and mortality were both studied, to assess whether their results align with (or contradict) those conclusions.
This exercise was prompted when we learned about a study that substantially increased rates of EIBF and SSC but did not lower mortality – leading us to question whether we had previously overestimated the benefits of these practices. After examining 24 randomized and quasi-experimental trials conducted across low- and middle-income countries, our headline view remains the same: the evidence is still consistent with substantial mortality reductions from EIBF and SSC. Additionally, we now have greater confidence that EIBF is both highly variable across settings and generally responsive to intervention.
Our aim was to pressure-test our prior work by seeking out contrary evidence: we knew that studies designed to produce changes in multiple determinants of neonatal health can’t “prove” the benefits of EIBF or SSC even if they raise rates of these practices and show mortality benefits [2]. But if package interventions consistently increase EIBF or SSC substantially without reductions in mortality, that would challenge our prior understanding.
To identify relevant evidence, we searched for trials that reported both mortality outcomes and rates of EIBF and/or SSC in intervention and control groups, ultimately identifying 24 studies meeting these criteria. These studies were mostly cluster randomized trials, largely based in South Asia, and highly heterogeneous in setting, intervention components, and design.
Across this set of trials, we found that interventions producing larger increases in EIBF rates generally also showed greater reductions in neonatal mortality. While correlation cannot establish causation, the pattern is consistent with the other evidence that we summarized in our previous report: EIBF involves biological mechanisms likely to reduce mortality, and there is strong observational evidence linking EIBF to lower mortality.
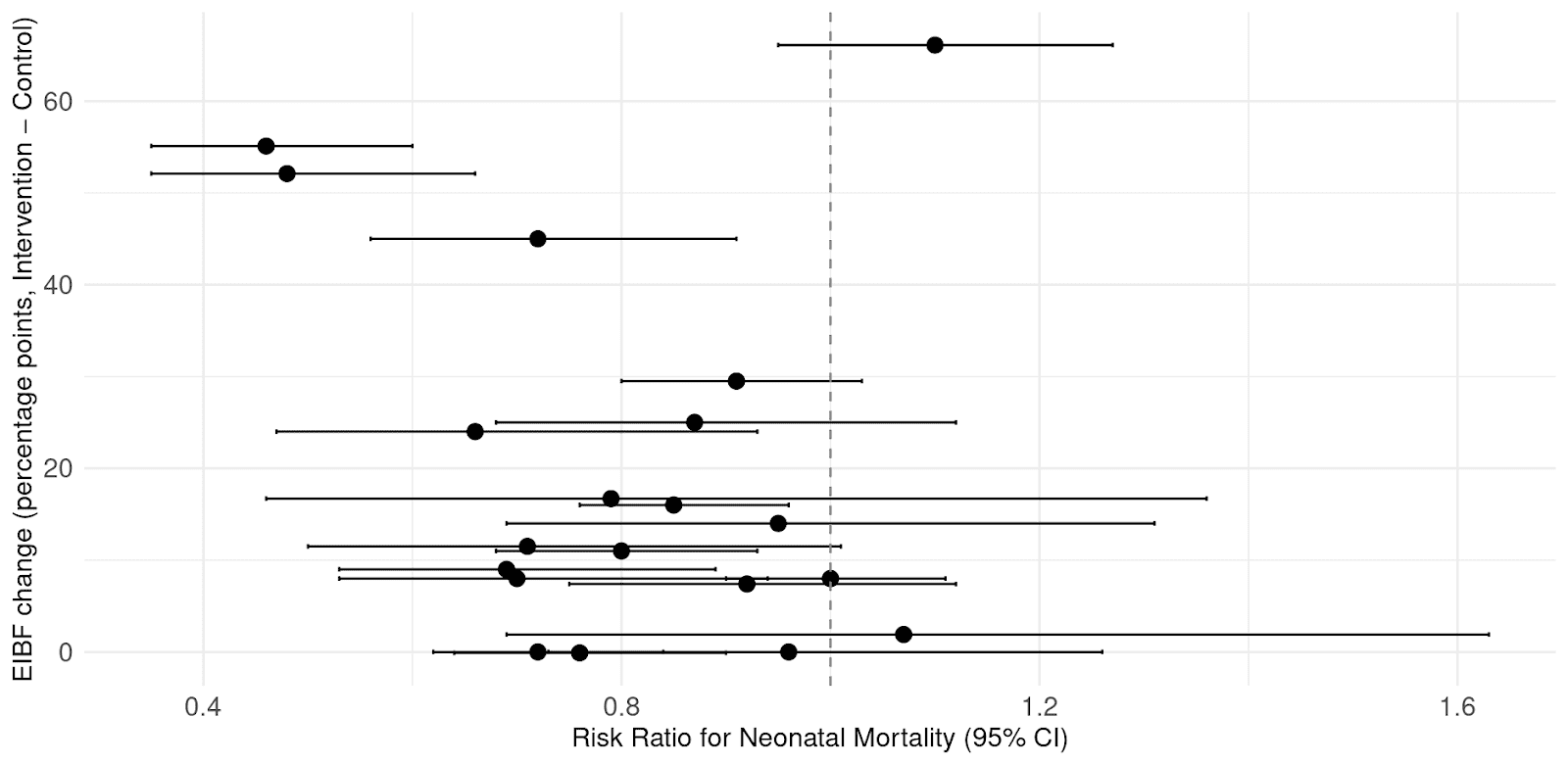
Correlation between neonatal mortality risk ratio and changes in EIBF among the trial arms we examined.
When we focus on the subset of randomized trials that increased EIBF by at least 10 percentage points, the reduction in mortality is substantial. Our meta-analysis, shown below, finds a 23% reduction in neonatal mortality (RR 0.77, 95% CI 0.65–0.91) among these studies. Observed mortality benefits are directionally consistent with EIBF and SSC being involved in mortality reductions and exceed what we would attribute to EIBF alone, suggesting additive or synergistic effects from other intervention components.

Meta-analysis of neonatal mortality in trials reporting a ≥10 percentage point increase in EIBF.
Important caveats remain. Most importantly, these interventions were not designed to isolate specific newborn care practices, so we cannot cleanly attribute the mortality benefits to EIBF or SSC. Many studies reported relatively modest increases in EIBF, which we wouldn’t expect to produce a strong mortality signal without other contributing factors. Next, because most included studies relied on maternal self-report for EIBF and SSC, rates of these practices could be overstated due to social desirability bias.
Even with these limitations, this review strengthened our views in a few ways. It provides further evidence that EIBF rates vary substantially between different settings and are often responsive to interventions (even when those interventions are not particularly focused on EIBF). Most importantly, it is consistent with our earlier conclusion that promoting immediate SSC and early breastfeeding is a promising and underappreciated opportunity to save newborn lives globally.
For more details, please refer to the longer report.
[1] Which we define here as “interventions designed to produce changes in multiple determinants of neonatal health”.
[2] Mortality reductions in such studies would be consistent with our understanding that EIBF and SSC save newborn lives, but attribution of the benefit to any specific practice impacted by the package would not be possible.
Join our email list to get occasional updates from us.